|
OVERVIEW OF DIABETES MELLITUS

|
HERE ARE THE TAKE-HOMES
FOR PET DIABETES
- DIABETES MELLITUS IS CAUSED BY A DEFICIENCY OF INSULIN. YOU ARE
PROBABLY GOING TO HAVE TO GIVE INJECTIONS OF INSULIN AS A REPLACEMENT.
(DON'T WORRY. IT'S EASIER THAN YOU THINK).
- The main symptoms of diabetes mellitus are excessive urination, excessive thirst,
excessive appetite, and weight loss. Treatment should control these symptoms.
- Watching for these symptoms is the best way to know how your pet is doing.
- THE STARTING INSULIN DOSE IS GOING TO BE BASED ON AVERAGES
AND WILL BE TWEAKED BASED ON TRIAL AND ERROR DEPENDING
ON BOTH TEST RESULTS AND CONTROL OF THE SYMPTOMS.
- YOU CAN SAVE A LOT OF MONEY IF YOU GET YOUR OWN GLUCOSE METER
AND LEARN TO DO BLOOD SAMPLING AT HOME (IT'S EASIER THAN YOU THINK).
- USING TOO LITTLE INSULIN IS A PROBLEM IN THE LONG TERM
BUT TOO MUCH INSULIN IS POTENTIALLY AN EMERGENCY IN THE SHORT TERM.
BE SURE YOU KNOW HOW TO RECOGNIZE HYPOGLYCEMIA AND WHAT TO DO ABOUT IT.
|
|
|
WHAT IS DIABETES MELLITUS?
In order to understand the problems involved in diabetes mellitus it is necessary to understand something of the normal body's sugar metabolism.
The cells of the body require fuel in the form of fat or sugar to conduct their daily activities. Some tissues can use either sugar or fat depending on circumstances and some tissues (such as the brain and nervous system) depend almost exclusively on sugar as fuel. Diabetes mellitus mostly involves the metabolism of sugar (in particular, a sugar known as glucose) so we will focus on the sugar part of the situation. Glucose comes from the diet in the form of starches and sugars that we eat.
Tissues cannot absorb glucose unless a hormone known as insulin is present. This special hormone, insulin, is produced by the pancreas as part of the body's natural blood sugar regulation. Insulin can be considered to be a key that unlocks the door allowing sugar in the bloodstream to enter the cells of the body. Once inside the tissues, glucose can be burned for fuel or stored but without insulin, the sugar stays in the bloodstream and cannot be used by the body.
|
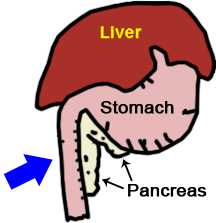
The pancreas is nestled along the stomach and small
intestine. It secretes digestive enzymes into the
small intestine but it also secretes hormones into
the bloodstream to regulate blood sugar.
(original graphic by marvistavet.com)
|
|
Chemical structure of glucose, our body’s main fuel source.
(Photo credit: public domain graphic via Wikimedia Commons)
|
|
Imagine you're in your home on lock-down and you need food.
You call a delivery service, they bring food,
you open your door and get your food.
You can eat the food right away or store it for later.
The system works.
Now imagine you can't open your door and are sealed in.
There is no way to access the food on your doorstep.
Inside with no way to get to the food, you begin to starve
and consume everything possible inside.
Outside food accumulates to a point it must be dumped.
In this analogy, insulin would be the key
that allows your door to unlock.
|
 (Photocredit: Teri Ann Oursler, used with permission) (Photocredit: Teri Ann Oursler, used with permission) |
|
IN THE DIABETIC ANIMAL THERE ISN'T ENOUGH INSULIN
In fact, there may be no insulin at all. Remember that insulin was the key to unlock the cell so that glucose could be brought inside. With no insulin, glucose cannot get in. Not only is glucose not being taken in and stored, but it is left floating around in the bloodstream in extremely high amounts. The body's tissues are starving and the bloodstream has plenty of glucose to feed them but without insulin, the glucose is unavailable.
SO WHAT SYMPTOMS RESULT FROM THIS?
Because there is no way to remove the glucose from the bloodstream, blood sugar levels are astronomically high. Normally, the kidney is able to conserve the bloodstream's glucose but its mechanisms are overwhelmed and glucose spills into the urine in high amounts. If we continue our food delivery analogy, all the undeliverable food must be dumped. In the body, glucose dumping happens in the kidney with extra glucose dumping in the urine. This process involves the use of a lot of water with the ultimate result being a lot of urine being produced to process all that glucose to dump. This translates into Excessive Thirst and Excessive Urination.
The tissues of the body are unable to access any of the glucose they need for fuel and are basically starving. Fat is mobilized and muscle is broken down to help feed the tissues but it does not do much good without insulin to bring fuel inside the cells. The patient shows Excessive Appetite because his/her body is in a state of starvation. Because the body is rapidly breaking itself down, Weight Loss is also a classic sign.
All the sugar in the urine presents a desirable growth medium for bacteria and Urinary Tract Infection is a common finding in diabetes mellitus.
In diabetic dogs (but not cats), a special type of cataract rapidly develops in the eye when glucose enter the lens of the eye in high amounts. Glucose normally feeds the lens of the eye but the amounts of glucose coming into the lens in the diabetic state are much higher. Excess glucose is converted to another sugar called sorbitol, which in turn attracts water. The excess water disrupts the clarity of the lens creating a diabetic cataract which leads to blindness in almost all diabetic dogs.
|

The diabetic animal will be very thirsty
and will make lots of extra urine.
(original graphic by marvistavet.com) |

(original graphic by marvistavet.com) |

Cataracts and blindness are almost
impossible to prevent in diabetic dogs.
(Photocredit: Public Domain Graphic via Wikimedia Commons) |
|
The main symptoms of Diabetes Mellitus are:
Excessive Thirst
Excessive Urination
Excessive Appetite
Weight Loss
|
|
IS IT LIKE THE HUMAN DISEASE? WILL WE NEED TO GIVE INSULIN SHOTS?
Dogs: Diabetes is most likely permanent and yes on the insulin shots.
Cats: Diabetes might not be permanent. Yes on the insulin shots if you want a chance at Diabetic Remission.
Diabetes mellitus is a classical disease in humans and most of us have heard some of the terms used in its description. In humans, diabetes is broken down into two forms: Type I and Type II. These are also referred to as "juvenile onset" and "adult onset" diabetes or "insulin dependent" and "non-insulin dependent” diabetes. In short, Type I is the type where the pancreas produces no insulin at all, and Type II is the type where the pancreas produces some insulin but not enough. Many pet owners wonder if dogs and cats have similar categories for their disease.
Virtually all dogs have "insulin dependent diabetes" and must be treated with insulin. There is no way around it. Their condition is very similar to the Type I diabetic human in many ways.
Most cats have "non-insulin dependent diabetes" at least to start. This suggests that some cats can get away without insulin injections and, indeed, some cats may qualify for oral options or temporary treatment with insulin. For cats, diabetes can resolve if we can re-activate the pancreas promptly.
Not all diabetic cats are similar to humans with Type II diabetes. Some diabetic cats, perhaps as many as 25%, have more severe hormone issues, such as acromegaly or Cushing's disease, that make them not only insulin dependent but difficult to regulate.
TREATMENT: GIVING INSULIN BY INJECTION
|
(original graphic by marvistavet.com)
|

(original graphic by marvistavet.com)
|
Since deficiency of insulin is the problem, it should not be surprising that giving insulin is the solution. You will need to learn to give injections, which is daunting to some owners at first, but almost everyone quickly becomes an expert.
|
First, an insulin type and dose will need to be selected. There are several types of insulins to select from and it is not possible to know exactly how much insulin your individual pet will require; trial and error is needed. Your veterinarian will make a guess based on what works for other cats and dogs and what has been reported in the literature. Most pets require injections twice a day, approximately 12 hours apart, in conjunction with a meal. Because overdose of insulin is potentially an emergency, it may be prudent to start with once a day insulin, just in case. If you like, discuss the pros and cons of each approach with your veterinarian.
Insulin has traditionally been given by syringe in a shot but insulin pens are proving more and more popular. The syringe method involves buying a box of syringes and a bottle of insulin, drawing up a measured amount of insulin and giving a shot. The pen involves applying a needle tip to the "pen," dialing a dose on the "pen," sticking the tip into the pet's skin and pressing a button on the "pen." Most people feel the pen method is much easier to perform but it may be difficult to find needle tips that are long enough for pet use as pet skin is much thicker than human skin. In some situations, the pen is used as a dispenser for the syringe as the pen cartridges may be more cost effective than bottles of insulin. Without video or first hand experience with insulin pens or syringes, it may be hard to visualize the difference. See our section on insulin administration for dogs or insulin administration for cats for details. Not all pet insulins are available in a pen format. Your veterinarian will instruct you regarding option.
|
Insulin and syringe
(Photocredit: Public Domain Image via Wikimedia Commons)
|
Some insulins are available from the neighborhood pharmacy and some kinds are available only through veterinary offices and veterinary pharmacies. Your veterinarian will either provide you with supplies or will give you the necessary prescriptions. If you are using syringes (instead of a pen) it is important to be sure the syringes and insulin concentration match. Insulin syringes are marked in insulin units (either “U-100” syringes for 100 unit/cc insulins or “U-40” syringes for 40 unit/cc insulins.) Whenever you receive more supplies, always double check these numbers.
A bottle of insulin, when stored properly, should last 6-8 weeks.
After that time it should probably be replaced.
|
(original graphic by marvistavet.com)
|
(original graphic by marvistavet.com)
|
Insulin syringes and insulin bottles are marked as U-100 or U-40. Always be sure the syringes and bottles match.
Never alter the insulin dose recommended by your doctor. To determine whether dose adjustments (or even a different type of insulin would be more appropriate), the pet will need a "glucose curve" where sugar levels are tracked over 10-24 hours. This can be done either by testing glucoses with a glucose meter every 2 hours or so or by using a continuous monitor such as a Libre Freestyle®. If a meter is used, it is best to sample glucoses in the pet's own home and send the values to the vet but the curve can certainly be performed in the vet's office. Note that stress and anxiety will alter blood glucose levels which means that values obtained at home will be more representative of the pet's situation.
For more details on glucose monitoring click here.
TREATMENT: ORAL AGENTS (CATS ONLY)
Some cats will qualify for oral treatment of their diabetes. There are two medications that might be employed for this: Bexagliflozin and Glipizide.
Bexagliflozin enhances the kidney's ability to dump extra glucose thus keeping blood sugar levels at lower levels. Lower blood sugar levels enables some recovery to occur in the pancreas and alleviates many symptoms of diabetes. On the flip side, only certain cats will qualify for use and there is potential for some very serious side effects so proper monitoring is crucial. Fore more details, follow the link above.
Glipizide is a human medication used to reduce glucose levels. It is not as strong as bexagliflozin but does not involve intense monitoring and does not have the same risk for complications. It is typically used for borderline patients or patients where insulin injections are simply not possible. Approximately 25% of cats will respond. For details, follow the link above.
DIET AND FEEDING
Regulation can generally be worked out on whatever diet the pet is eating but there are some diets and feeding strategies that are helpful. For dogs, high fiber/low fat diets are preferred as they slow the absorption of sugars in the diet and help maintain a more regulated blood sugar level. Fiber also seems to make the body's tissues more sensitive to insulin which also helps with regulation. Rewards are often employed to facilitate the insulin injection experience but these calories can add up and interfere with regulation so be sure your veterinarian is aware of all food items. Diabetic dogs are best fed in two meals, approximately 12 hours apart. After they have been seen to eat their food, their insulin dose can be given.
For cats the strategy is different. First, cats seem to do best fed in multiple small meals daily so they should be allowed access to food at all times. Second, the high protein/low carbohydrate diets seem to be the most conducive to regulation. There are specific prescription diets in both canned and dry formulations that are designed to assist diabetic cats.
For more details on handling diet and feeding, click here for cats and here for dogs.
WHAT ABOUT HOME GLUCOSE TESTING?
Home glucose monitoring has many benefits: glucoses are monitored in the comfort of the pet's own home without alterations from vet visit anxiety, a lot of money can be saved by monitoring at home, questions about glucose status can be quickly answered and addressed. There are two ways to monitor glucoses at home: Continuous monitoring and glucose meter.
|
CONTINUOUS MONITORING
Continuous monitors have changed the way diabetic pets are monitored. A sensor with a tiny needle is implanted on the pet and paired wirelessly to either a phone or a reader. It reads tissue glucose levels constantly and reports its data to the device or your choice as well as to an internet portal where your veterinarian can access it. The sensor set up lasts up to 2 weeks and typically costs less than an in-house glucose curve run in the hospital. This is a fantastic option when it is time to get get a glucose curve. If one simply wants to spot check a glucose level, one will need a glucometer and you will need to be able to take a blood sample from your pet.
|
 Cat with Freestyle Libre sensor in place. Cat with Freestyle Libre sensor in place.
(Graphic by marvistavet.com) |
GLUCOMETER/GLUCOSE METER
|
Many pet owners like to check glucose levels prior to insulin injections on a daily basis or simply want the ability to check a glucose level if there is a concern for hypoglycemia. For these situations, a glucometer is needed. Human meters can be obtained at any drugstore but we recommend getting a veterinary meter as the calibration is different. AlphaTrak is a popular brand but there are presently several other brands available.
The meter kit will contain measuring strips, solutions for calibration, and a spring-loaded lancet device for taking blood samples (usually from the ear margin). For details please visit the Diabetes Monitoring section of this library. Taking single drop blood samples turn out to be easier than you might think and video links are provided in the monitoring section. Still, not every pet is amenable to blood sampling and we do not want anyone getting bitten or scratched.
If you choose to use a glucometer at home, be sure to keep a log of when your pet was fed, when insulin was given, and what the glucose levels were that you found. (There are many phone apps to assist with this). Bring this log to your veterinarian when you come for check ups. Glucose levels obtained prior to the first insulin administration of the day are particularly useful. Your veterinarian will also be particularly interested in signs associated with poor regulation: excessive thirst, excessive urine production, excessive appetite, and weight loss.
|
 (original graphic by marvistavet.com) (original graphic by marvistavet.com) |
If your pet is too sensitive for a valid glucose curve at the vet’s office and you do not think you are up to blood sugar testing at home, the fructosamine blood test may be particularly useful. Again, this test looks at average glucose levels so wide fluctuations will not be discovered but at least there is a monitoring option for this situation.
HYPOGLYCEMIA AND OTHER THINGS TO WATCH FOR
|
The most serious problem to watch for is hypoglycemia (low blood sugar). This results from a mismatch in food consumption and insulin dose. If the dose is too high you can get hypoglycemia. If the pet doesn't eat, you can get hypoglycemia. Your pet may look simply tired, weak, or sleepy. If he/she is roused, he will seem drunken or may not be able to fully come to alertness. This can be an emergency and can progress to seizures so it is good to know what to do at home to prevent disaster.
If your pet appears wobbly or drunken, his/her blood sugar level may have dropped too low. This occurs after an insulin overdose. First try to get your pet to eat. If the pet will not eat, administer light Karo syrup, honey, or even sugar-water at a dose of one tablespoon per 5 pounds. The sugar will absorb directly from the mouth; swallowing is not necessary. If no improvement occurs, immediately see your veterinarian for emergency treatment. When your pet is more stable, a glucose curve will be needed to determine why this happened and what a more appropriate insulin dose might be.
It is best to know that your pet has recently eaten before giving the scheduled insulin dose.
|
(original graphic by marvistavet.com)
|
OTHER REASONS TO RETURN TO THE VET
Bring your pet in for a re-check exam and testing if you note any of the following:
- the pet seems to feel ill.
- the pet is losing weight.
- the pet has a ravenous appetite or loses its appetite.
- the pet seems to be drinking or urinating excessively.
- the pet becomes disoriented or groggy.
It is important for diabetic pets to have their teeth cleaned annually. Dental tartar seeds the body with bacteria and when blood sugar levels run high, infections in important organs can take root. The kidneys and heart are particularly vulnerable.
SOME PETS ARE DIFFICULT TO REGULATE
Some pets seem to require re-regulation frequently. There may be an underlying reason to sort out. Here are some possibilities should your pet seem to fit in this category:
- Improper administration of insulin. If possible, have your doctor observe you giving the insulin to your pet. Another possibility is that your insulin may be out of date.
- Rapid insulin metabolism. Insulin wears off quickly in some animals. Your pet may require a different type of insulin or even additional injections during the day.
- Insulin overdose may actually lead to elevated glucose levels (and clinical signs of diabetes mellitus). In this situation, too much insulin brings the blood glucose too low and other hormones respond to bring it back up (and generally over-do it).
- Steroid administration (such as prednisone, prednisolone etc.) will interfere with insulin.
- Progesterone, a female hormone, also interferes with insulin. Unspayed female diabetics should be spayed once they are sufficiently regulated.
For more details on trouble with regulation, please see the section on The “Hard To Regulate Pet” in this center.
LINKS
For further information you may wish to visit:
www.felinediabetes.com
www.caninediabetes.org
A Pet Diabetes Mailing List is also available. To subscribe, visit their web page:
www.caninediabetes.org/pdorg/mailing_list.htm

Page last updated: 4/9/2025
|